The information presented in this case study was submitted by the identified provider and reviewed by the Unyte Clinical Team. Modifications to the text have been made solely for the purpose of enhancing comprehension and clarity for the reader’s benefit, and were carefully applied while ensuring the accuracy and integrity of the original submission. Unyte Health makes every effort to use updated terms and inclusive language, this case study retains the author’s original descriptions to be most sensitive to the client’s identity and preferences.
About the Provider
Name: Frances McBride
Disciplines/credentials: Doctor of Health Administration, Licensed Professional Counselor, Licensed Substance Abuse Treatment Practitioner, IFS Level 1 Trained
Modalities: Safe and Sound Protocol (SSP), Rest and Restore Protocol (RRP), Internal Family Systems (IFS)
Client Background
Name: Elizabeth (pseudonym)
Age and Gender: Woman, she/her/hers
Program Delivered: IFS in combination with SSP and RRP
Elizabeth initially arrived at the office without an appointment, appearing in severe distress. After assessing for safety, an appointment was set for the following day.
The evaluation took place in an office setting, with Elizabeth reporting a range of troubling symptoms that developed over the past six months, including headaches, irritable bowel syndrome, decreased appetite, trouble concentrating, difficulty sleeping, excessive sleep, low motivation, and isolation from others. A significant concern leading to this evaluation was Elizabeth’s expression of suicidal ideation, stating, “I would rather go to sleep and not wake up.” Compounding her distress were personal and familial challenges, including her military service of eight years, a recent relationship of three months, and the emotional burden of her little sister’s suicide attempts a few years ago, as she was blamed to be the reason. The recent diagnosis of cancer in her last living grandparent further exacerbated Elizabeth’s emotional turmoil.
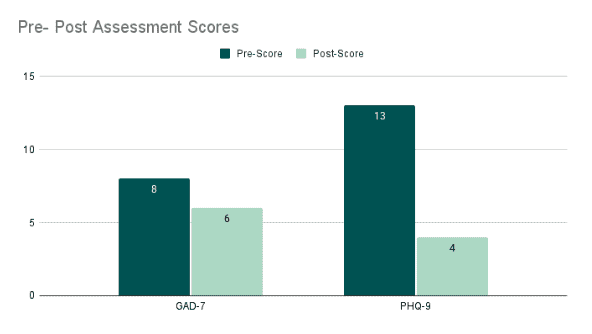
During the assessment process, the provider employed a variety of standardized measures to gauge Elizabeth’s mental health status comprehensively. The Clinically Useful Depression Outcome Scale (CUDOS) yielded a score of 25, indicating a moderate level of depressive symptoms. Additionally, Elizabeth completed the PCL-5, resulting in a score of 21, with responses for alterations in arousal and reactivity falling below the diagnostic threshold. The GAD-7 assessment revealed mild anxiety, as indicated by scores ranging between 5-9. The PHQ-9 indicated that Elizabeth’s symptoms were somewhat hindering her functional capacity, and Elizabeth candidly reported thoughts of suicide or self-harm. Notably, the provider observed that Elizabeth appeared to underrate her symptoms, as her emotional state during the initial visit conveyed a more profound level of distress than reflected in her responses. Despite the inner turbulence that limited early access to clarity and confidence, self-energy flickered through: a wish for inner peace, a desire to “explore relationships and how to be a loving, caring, compassionate human being,” and occasional contact with a wise, benevolent inner voice encountered in nature (“God is everything and I am that”). Such moments were regularly interrupted and silenced by the harsh critic: “Coming back to myself is a letdown.”
Background
Exploring Elizabeth’s family history provided crucial context for understanding her current emotional state. Elizabeth recounted her childhood experiences, particularly highlighting her father’s struggles with alcoholism, which ultimately led to a recent liver transplant due to excessive drinking. She described the atmosphere in her home, where she witnessed domestic violence against her mother, and felt a pervasive lack of emotional support and closeness among immediate family members. This history has contributed to a longstanding perception of being unloved or unimportant within her immediate family. Elizabeth mentioned feeling overwhelmed at work, where she was in a leadership role responsible for over 20 individuals, which amplified her stress. The added pressure of having to make decisions, even for simple matters, underscored the weight of her responsibilities, particularly as she prepared for an upcoming deployment.
Reason for Seeking Services
The clinical impressions derived from the evaluation suggested a diagnosis of moderate depression, with possible post-traumatic stress disorder symptoms that do not fully meet the diagnostic criteria. Elizabeth’s reports, along with the results from standardized tests, indicate that her symptoms of depression and anxiety were significantly impacting her daily functioning. Given the expression of suicidal ideation, it was imperative to closely monitor Elizabeth’s risk level and provide appropriate follow-up to ensure her safety.
Introduction of IFS
Throughout interactions, Elizabeth appeared introspective, indicating a willingness to delve into the underlying beliefs driving her current behaviors. The provider introduced the IFS Model, aiming to help Elizabeth identify internal parts that might be holding onto the responsibility of others. This approach was met with curiosity and openness from Elizabeth, who seemed eager to understand how these internal dynamics could be influencing her actions and emotional state.
During the sessions, Elizabeth shared a significant legacy burden centered on the belief that it was her responsibility to help financially and solve problems within the family and military. This burden manifested in tangible ways, such as Elizabeth contributing to her mother’s car payments and covering her father’s cell phone and utility bills. The discussion revealed that these financial obligations have been a longstanding pattern, potentially rooted in deeper familial expectations or learned behaviors. Elizabeth expressed a sense of duty and obligation, yet there was also an underlying tone of fatigue and frustration, suggesting that these responsibilities might have been weighing heavily on her.
The provider facilitated a deeper exploration into the parts of Elizabeth that held these burdens, employing the IFS Model to guide this introspection. Elizabeth appeared to resonate with the concept of internal parts, acknowledging that different aspects of her psyche might have been at play in perpetuating these responsibilities. The provider’s approach encouraged Elizabeth to consider how these parts developed and what needs they might have been fulfilling. Through these discussions, Elizabeth began recognizing the possibility of shifting these burdens and exploring new ways of interacting with her family and military personnel.
Implementation of the Safe and Sound Protocol (SSP) and Rest and Restore Protocol (RRP)
The provider began the SSP in the office, initially for 15 minutes at a time with over-the-ear headphones. Before and after listening therapy, the provider asked Elizabeth to check in with her parts and bodily sensations. Over the course of two weekly sessions, Elizabeth demonstrated progress by gradually increasing the duration to 30 minutes. This gradual approach aligned with the metaphor “slow is fast,” emphasizing the benefits of taking a measured pace for effective integration of the therapy. The provider explored Elizabeth’s current home environment and listening devices, in which she was granted remote delivery of the RRP. This therapy aimed to help Elizabeth relax in the evenings, thereby promoting better sleep. Elizabeth seemed optimistic about incorporating this new component into her routine, understanding its potential benefits for relaxation and sleep enhancement.
Response
The provider noted that Elizabeth’s PHQ-9 scores had decreased, indicating minimal or no depression. While Elizabeth admitted that her symptoms made functioning somewhat difficult at times, she expressed relief at the substantial progress made. Elizabeth shared the feelings of responsibility and the metaphorical burden she felt had been lifted from her shoulders and other areas of her body. This revelation seemed to correlate with Elizabeth’s reported decrease in anxiety levels, as measured by the GAD-7 scale. Elizabeth’s scores ranged from 5 to 9, which fell within the category of mild anxiety. Importantly, Elizabeth noted that her anxiety symptoms were not significantly impacting her ability to function in daily life, which was an encouraging development.



 © 2026 Unyte Health US Inc.
© 2026 Unyte Health US Inc.