| By Rebecca Knowles, OTD, OTR/L, RYT, and Susanna Coss Reviewed by Unyte Clinical Team and Stephen Porges, Ph.D. |
What is the vagal paradox?
As the most influential nerve in the parasympathetic system, the vagus nerve (CN X) plays an important role in supporting and restoring homeostasis, known as the “rest and digest” part of the autonomic nervous system. The vagus nerve helps to slow heart rate, improve breathing, and share information between bodily organs and the brain, helping the body adjust to its environment. In this state, the brain and body work together to help us think, feel, and connect better with others.
However, the vagus nerve has a second, paradoxical (or seemingly contradictory) role in shutting down the body in response to threat. The body’s detection of threat can come from physical conditions, such as hypoxia (low oxygen), traumatic experiences, or even chronic stress. When the body feels threatened, the vagus can either remove the “brake” on the heart’s pacemaker, allowing it to beat faster, or potentially slow the heart rate so much that it reduces the amount of oxygen in the blood. It can also lower blood pressure dramatically, enough to cause dizziness or even fainting. The vagus nerve can also profoundly influence the digestive system (e.g. triggering diarrhea in response to stress).
Through decades of research, Polyvagal Theory has been cited in thousands of publications across disciplines. Polyvagal Theory explains how the brain and body have adapted over a long period of time. The vagus nerve itself has changed, in location and function, to serve these two roles alongside the sympathetic system, which is commonly known as the “fight or flight” response. Together, these poly (many) roles of the vagus nerve help us survive and, even better, to thrive in the modern world.
The Evolution of Polyvagal Theory
Since its original publication in 1995, Polyvagal Theory has been well-received in academic science and has been cited in about 20,000 peer-reviewed articles with almost universal acceptance.
As is often the case in academia, a few scientists have shared criticisms of Polyvagal Theory. In his new paper, titled The vagal paradox: A polyvagal solution, Dr. Porges directly addresses them. He notes that they do not accurately represent the theory, but rather mislead by offering straw man arguments and debate against misinterpretations of his research. He identifies specific examples of these and contrasts them with the actual statements of the Polyvagal Theory in published literature.
Dr. Porges has welcomed the opportunity to evolve, refine and clarify the scope of the theory. His latest publication is a summary of these discussions, diving deep into questions about how the human nervous system evolved, how it functions today, how to measure change, and implications for practice. His goal is to enable and encourage a fair and productive discussion that revolves around genuine points outlined in the Polyvagal Theory, thereby mitigating the impact of fallacy-based arguments.
Six Key Takeaways
The autonomic nervous system (ANS) states are hierarchical and antagonistic.
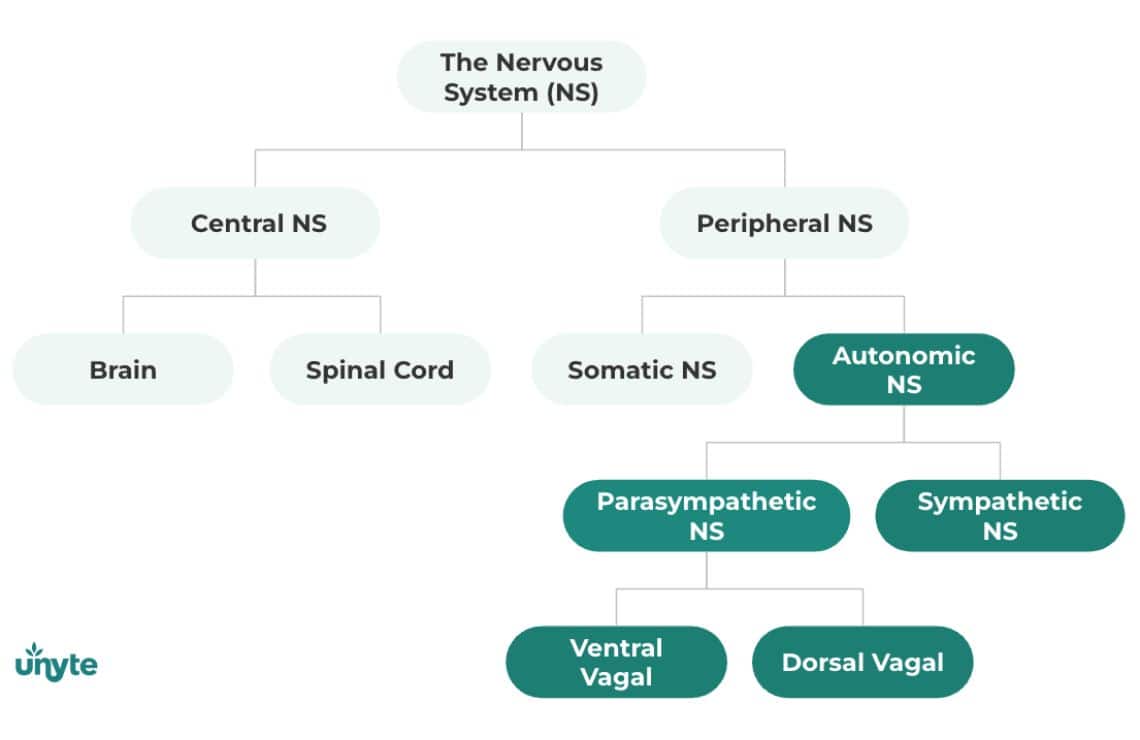
A simple way of thinking about the autonomic nervous system is to consider the two states — sympathetic and parasympathetic — as opposites, or antagonists, toward each other. When one state takes the lead, the other backs off.
Polyvagal Theory describes the complexity of the nervous system not as two states working against each other, but rather three states guided by two branches of the vagus nerve in the parasympathetic system (the vagal paradox). The order in which these states respond is reflected in both how the nervous system evolved (phylogeny) and how the nervous system develops from a single cell to an infant (embryological development). This view is closer to how the body actually responds to stress in the real world, and what presents in the clinic or therapy office.
This hierarchical pattern is a core principle in Polyvagal Theory, but isn’t the only way the ANS works. The nervous system is complex and dynamic, constantly responding to cues from the internal (body systems and organs, feelings like hunger) and external worlds. While it generally follows the order described by Polyvagal Theory, the ANS responds both hierarchically and antagonistically to keep us alive.
Evolution gives us clues about how the nervous system works today.
The social engagement system includes muscles in the face and head that help us communicate and connect with others. Different from reptiles, humans can coordinate suck, swallow, breathing and speech. We also have special nerves that regulate the middle ear muscles, allowing us to better perceive the calming frequencies of human voice and distinguish it from threatening, low-frequency sounds of predators and high-frequency sounds of danger. This adaptation is the foundation of the Safe and Sound Protocol (SSP), which helps to regulate the nervous system, improve auditory processing, and help us connect better with others.

Discover the Safe and Sound Protocol
Created by Dr. Stephen Porges, the Safe and Sound Protocol (SSP) is a powerful listening therapy based on the science of Polyvagal Theory.
Studying how the vagus nerve and other structures in the social engagement system have changed over time helps scientists understand how humans function in the world today.
Amazingly, the pattern of human embryological development often mirrors evolution. This map of human history in the womb gives clues about how the nervous system has changed over time. Along with other observations of behavior and anatomy, this is what led to the development of Polyvagal Theory.
In The vagal paradox: A polyvagal solution, Dr. Porges clarifies that Polyvagal Theory does not claim to explain how evolution works. Instead, it looks at well-established patterns in the evolutionary transition from ancient (and extinct) to modern species, where structures of the social engagement system first began to emerge in mammals about 220 million years ago. Getting too caught up in the complex process of evolution, especially in differences between ancient and modern species, can distract from the core principles of Polyvagal Theory and misses the point.
In many ways, comparing the nervous systems of different species from today and from the past builds the foundation for understanding the human ability to trust, feel safe and co-regulate with others.
There’s much we still don’t know — and may never know — about human history. This knowledge is changing all the time as we develop better tools, like molecular techniques, rather than relying on fossil records. To date, scientists haven’t been able to look closely enough at the timeline and species referenced in Polyvagal Theory to be of much use.
The vagus nerve has changed in location and function.
Conceptually, the vagus nerve is a conduit with fibers emerging from different areas. Imagine the vagus like a highway, with many cars (fibers), each coming and going from different locations to do different things. Central to Polyvagal Theory and the SSP is a division of the vagus motor fibers, which originate in ventral and dorsal areas of the brainstem and have different roles in regulating the nervous system (the vagal paradox).
This specialization is made possible by the changing location of a newly emerging ventral branch of the vagus nerve within the brainstem. There are many examples of evidence for this change, both looking back and at the present.
For example, the ability to nurse is observed in the very earliest mammals, even before modern reptiles evolved. Scientists can also confirm the unique roles of the ventral and dorsal vagus using electrical stimulation to elicit the expected response (e.g. stimulating the dorsal vagus in rabbits slows heart rate). More plainly, the role of the ventral vagus in the social engagement system can easily be seen in the co-regulation between a mother and infant: the soothing, melodic voice of a mother predictably regulates their infant’s heart rate (Kolacz et al., 2021).
We can similarly understand how the vagus fibers became more myelinated over time, becoming even faster and stronger, through autopsy data. We can also measure the coordination of breathing and heart rate through respiratory sinus arrhythmia (RSA), another feature unique to mammals. Some have questioned Polyvagal Theory because a similar breathing-heart rate pattern can be observed in other vertebrates. Again, this criticism misses the point that unique to mammals (not in other vertebrates), the respiratory rhythm in heart rate (i.e. respiratory sinus arrhythmia) are guided by myelinated vagal fibers emerging from the nucleus ambiguus (i.e. origin of the ventral vagus). In other vertebrates, respiratory-heart rate interactions are guided by vagal fibers originating in the dorsal nucleus of the vagus. There is plenty of evidence in animal and human research to confirm, consistent with Polyvagal Theory, that the myelinated ventral vagus helps humans coordinate breathing, sucking, vocalizing, and heart rate to nurse and to socially engage with others.
When newer patterns don’t work, the nervous system resorts to its old ways.
When the ventral vagus is not able to resolve a stressor, the sympathetic system takes the lead. If the stress is still not resolved, the nervous system resorts to the dorsal vagus for help.
Evidence for this hierarchical response pattern is basically evolution in reverse, known as the Jacksonian principle of dissolution. It’s difficult to rely exclusively on evolution to prove this pattern because of gaps in our historical knowledge; however, this pattern can be observed in modern clinical settings. For example, the order of changes in brain function following brain injury or illness follow the same predictable, hierarchical pattern described in Polyvagal Theory. This pattern is also consistent with the order of human development. Some critics of Polyvagal Theory inappropriately draw conclusions from modern reptiles that evolved long after mammals already had a functioning ventral vagal/social engagement system, and lose sight of development and what is clearly seen in embryology and autonomic reactions in real-life situations.
One instance of real-life evidence comes from observing heart rate and the breathing-heart patterns of preterm infants.
In high-risk preterm infants, when the breathing pattern in heart rate (respiratory sinus arrhythmia) is dampened in response to life’s challenges, their heart rate rapidly increases before dramatically dropping. When the ventral vagus isn’t fully able to keep the heart rate in homeostatic bounds, the sympathetic system takes charge, spiking the heart rate. The dorsal vagus then jumps in to slow the heart rate back down, sometimes to dangerous, life-threatening levels. This is another example of the body following the same hierarchical pattern explained by Polyvagal Theory.
Dorsal doesn’t always equal defense.
While the dorsal vagal state is often thought of as the last line of defense, associated with shutting the body down to support the “freeze” state, it also works alongside the ventral vagus to support a well-balanced body.
When we’re healthy and safe, the dorsal vagus is responsible for ensuring that gut and digestive processes stay in check. If the dorsal vagus becomes too active in response to threat, it can lead to issues, such as ulcers (sores in the stomach or intestines) or irritable bowel syndrome.
Preview: A special conversation featuring Stephen Porges and Gabor Maté
Drs. Porges and Maté discuss safety in healing, healthcare, academic science and more in this nearly hourlong conversation, titled Humanity and Sociality: Healing Through Safety, Connection and Compassion. (Subscription required.)
How exactly the ventral and dorsal vagus contribute to the regulation of heart rate and blood pressure hasn’t been fully figured out. However, the dorsal vagus appears to take a back seat. On occasions when the ventral vagus is unable to keep the body regulated, the dorsal branch may work as a backup, sometimes overcompensating, which can disrupt blood pressure and slow the heart to dangerous levels.
The role of the dorsal vagus changes based on situations, health conditions, and the influence of the ventral vagus.
The ventral vagus is a window into understanding health and well-being.
The ventral vagus acts like a braking system for the heart, helping the nervous system adaptively respond to challenges. This braking function is an indication of how well-equipped the body is to cope with stress.
Our hearts are wired to beat faster than they do at a resting state. The ventral vagus helps keep the heart rate slow by acting as a “vagal brake.” This brake helps the heart match what’s going on in the environment and meet energy demands.
Researchers measure how well this brake works using something called vagal efficiency, which takes into account breath, heart rate, and the rhythmic relationship between them. Vagal efficiency is measured under changing situations, such as posture adjustments, to explore how the vagal brake adapts to challenges.
When the vagal brake isn’t working efficiently, research suggests that it leads to features of dysautonomia, as well as an increased risk for mental health challenges, such as anxiety and depression. Unsurprisingly, poor vagal efficiency has been observed in individuals with a history of trauma.
The influence of the ventral vagus on overall well-being highlights the need for therapies designed to improve vagal efficiency, in turn boosting nervous system resilience and flexibility.
What else does this mean for the Safe and Sound Protocol (SSP)?
Use the Body Perception Questionnaire, both in practice and research.
The Body Perception Questionnaire (BPQ) was developed to measure body awareness and autonomic reactivity through the lens of Polyvagal Theory. It’s often difficult and expensive to use physiological measures, such as heart rate monitors or skin conductance tests, to measure autonomic state. The BPQ is a more accessible alternative, using a client’s self-report to track autonomic symptoms.
The BPQ has been further validated in the lab and in other studies regarding the impact of adversity on mental health symptoms. SSP providers should consider using the BPQ as a pre- and post-program assessment with adult or adolescent SSP clients. The BPQ can be found in Unyte Assessments and administered digitally, in person or remotely.
Send cues of safety through both top-down and bottom-up approaches.
Neuroception, different from perception, is a subconscious process of the nervous system that evaluates cues from inside and outside the body as safe, dangerous, or life-threatening, which then trigger an autonomic response. For example, humans respond to pain by looking for the cause and attempting to avoid it. Even plants and other organisms without a nervous system have a form of neuroception, where their cells identify and respond to stressors at a cellular level.
The human response is much more sophisticated: we can respond not only to danger, but to safety in relationships, which shifts us into a calm state. This ability relies on both top-down (brain, thinking) and bottom-up (body, feeling) mechanisms. SSP providers should continue to use cues of safety through their voice and facial expressions, paired with psychoeducation, behavioral or talk therapies, or other top-down strategies to support and enhance the process of SSP delivery.
Integrate the five primary principles of Polyvagal Theory into your practice.
This recent publication has clarified some specific questions about Polyvagal Theory, alongside a summary and definition of the five primary principles. These can be used to explain trauma to clients, develop strategies for regulation, and build resilience and capacity in both clients and providers. You can also use the details in The vagal paradox: A polyvagal solution to be well-informed on the origins and evidence for Polyvagal Theory, and to prepare to respond to misunderstandings or misrepresentations of its scope.
There is a strong and growing evidence base for the SSP beyond Polyvagal Theory.
Although Polyvagal Theory forms the foundation of the SSP, there is a growing body of clinical trials and real world evidence that further our understanding of how and for what populations the SSP is most effective. There is also parallel research beyond Polyvagal Theory on how music can be used therapeutically to influence neuroplasticity and autonomic function.

Free Webinar: Exploring Polyvagal Theory, Interpersonal Neurobiology and the SSP with Dr. Stephen Porges and Dr. Tina Bryson
Linked by a shared passion for Polyvagal Theory, Drs. Porges and Bryson discuss central ideas of interpersonal neurobiology, including the mind, brain and interpersonal relationships in the context of the SSP through a deep-dive of neuroception and regulation.
Summary
Dr. Stephen Porges’ multidisciplinary work on Polyvagal Theory and the Safe and Sound Protocol (SSP) continue to influence the work of other scientists and clinicians, creating a ripple effect around the world. We’re grateful for this latest research publication, as well as the impact Polyvagal Theory has made and will continue to have on our knowledge of how the body works.
References
Kolacz, J., daSilva, E. B., Lewis, G. F., Bertenthal, B. I., & Porges, S. W. (2021). Associations between acoustic features of maternal speech and infants’ emotion regulation following a social stressor. Infancy : the official journal of the International Society on Infant Studies, 27(1), 135–158. https://doi.org/10.1111/infa.12440
Porges, S.W. (2023). The vagal paradox: A polyvagal solution. Comprehensive Psychoneuroendocrinology, 16, 100200. https://doi.org/10.1016/j.cpnec.2023.100200



 © 2025 Unyte Health US Inc.
© 2025 Unyte Health US Inc.