Associate’s Name & Discipline:
Mark L. Prohaska, Ph.D. (Director and Primary Therapist), Heather C. Miller, B.S. (Clinical Coordinator and Focus System Provider), Jodi C. Coon (Focus System Provider).
Name of Organization:
Neuropsychology Clinic, P.C.
Abstract:
N, a 7-year-old boy was brought in for ADHD-like symptoms reported by teachers and family. N’s performance on formal testing was not consistent with an ADHD diagnosis: results of executive functioning measures and his sensory profile yielded results that suggested underlying sensory processing deficits and delays. The Focus System was used in conjunction with Cognitive Behavioral Therapy, and after 5 months, the client saw gains of up to two years in academic testing, and an analysis of the DSM-V Symptom scales revealed an endorsement of symptoms that no longer meet criteria for any of the ADHD subtypes.
Client:
“N”, a 7-year-old male, in 1st grade
Background:
When first evaluated, N was a 7-year-old, male in the 1st grade. He lived with his biological parents and 10-year-old brother. He got along well with his peers, though was sometimes selfish and did not share well. He was described as being artistic and creative and enjoyed riding his dirt bike. Family history included ADHD (mother, grandfather).
Presenting Problem & Initial Findings:
N was initially evaluated for cognitive and behavioral symptoms of inattention, hyperactivity, and emotional dyscontrol.
His problems were particularly evident in the classroom, where his teachers commented that he had significant problems maintaining his focus and concentration and staying on task. Although there were no behavioral issues in the classroom, N did not seem to retain information presented in class, often failed to get his work done, and frequently left items blank on tests.
His mother observed that he got his numbers and letters confused and that it was hard to get him to sit down and do his homework, which took much longer to complete than it should. N would become easily frustrated and had frequent “meltdowns.” He was very distractible and often failed to follow through with instructions. Additional symptoms included poor fine motor skills (e.g., unable to tie his shoes), oral sensory seeking (e.g., fingers in mouth, chewing on clothing), and drooling.
Results of our evaluation, estimated N’s level of overall intellectual ability to be in the average range. Evaluation of academic achievement revealed significant relative weaknesses in sight reading, phonetic decoding, and both reading and writing fluency. N’s performance on formal testing was not consistent with an ADHD diagnosis and results of executive functioning measures and his sensory profile yielded results that raised underlying sensory processing deficits and delays in frontal system development as more likely etiologies of his presenting symptoms.
Therapeutic Goals:
Show improvements in
- higher order attention and executive abilities
- processing speed
- phonetic decoding
- reading skills
- sensory seeking behaviors
Unyte-iLs Program Used:
The Focus System: Sensory Motor Program 1-hour-sessions, three times per week, in clinic.
Other Interventions Used:
Cognitive-Behavioral Therapy (CBT) focused on specific difficulties identified in our assessment and over the course of therapy.
Post-treatment Evaluation:
Pre- data was collected on in December and post- data was collected in May.
At baseline, on the Wechsler Abbreviated Scale of Intelligence-II (WASI-II), N obtained an estimated Full Scale IQ of 101 (average range). An analysis of his index scores revealed equally balanced verbal and nonverbal abilities. N’s post-treatment performance on this measure yielded similar results.
| WASI – II | ||||||||
| Subtest | Raw | T-score | Scale | Sum of T-scores | CompositeScore | %ileRank | Confidence Interval (95%) | |
| Block Design | 15 | 52 | Verbal | 109 | (99) 107 | 68 | 100-113 | |
| Vocabulary | 20 | 52 | Nonverbal | 95 | (102) 96 | 39 | 89-104 | |
| Matrix Reasoning | 8 | 43 | Full Scale | 204 | (101) 102 | 55 | 96-108 | |
| Similarities | 21 | 57 | ||||||
| Confidence Level (IQ = 102 ) | Difference | Raw | Significance | Base Rate | ||||
| 90% | 68% | VCI>PRI | 11 | .15 | 15-20 | |||
| 102-103 | 102-103 | VCI<PRI | ||||||
*pre-treatment scores are in parentheses
N’s post-treatment performance on academic achievement measures revealed notable improvements in his grasp of phonics (25-points; <1.0 to 2.7 grade level), oral reading fluency (13-points; <1.0 to 1.9 grade level) and spelling (12 points; 1.0 to 2.1 grade level). With the exception of writing fluency, N’s performance in these areas is now generally consistent with or above his grade level.
| WIAT-III | Standard Score | Percentile | Grade Equivalent |
| Reading | (90) 103 | 58 | |
| Word reading | (87) 95 | 37 | (1.1) 1.8 |
| Pseudoword Decoding | (82) 107 | 68 | (<1.0) 2.7 |
| Reading Comprehension | (105) 103 | 58 | (1.7) 2.3 |
| Oral Reading Fluency | (83) 96 | 39 | (<1.0) 1.9 |
| Written Language | (82) 92 | 30 | |
| Alphabet Writing Fluency | (80) 87 | 19 | (PK.7) 1.0 |
| Spelling | (90) 102 | 55 | (1.0) 2.1 |
| Sentence Composition | (87) 94 | 34 | (1.1) 1.8 |
*pre-treatment scores are in parentheses
The IVA Continuous Performance Test is a computerized task specifically developed to assist in the diagnosis of ADHD. At baseline, N demonstrated intact response control for both auditory and visual information, with his full scale response control quotient falling in the high average range. He likewise demonstrated intact visual and auditory sustained attention and focus, though an isolated deficit in response time for visual targets, a pattern that was atypical of ADHD. N’s post-treatment performance on this measure revealed improvements in visual response time, with all of his attention scales now falling in the average range.
| IVA Continuous Performance Test | ||
| Attention | ||
| Baseline | Post-Focus System Rx | |
| Full Scale Quotient | 83 | 98 |
| Auditory | 96 | 104 |
| Visual | 76 | 93 |
* Lower scores reflect greater deficits
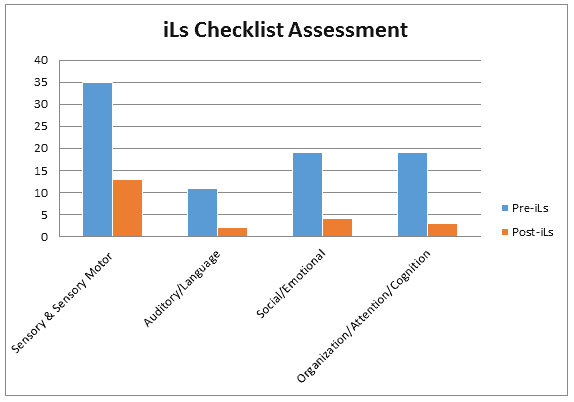
N’s mother completed the Focus System checklist at baseline and post-treatment. Her observations suggest notable improvements in all areas over the course of treatment.
*Higher scores reflect greater deficits
An analysis of the DSM-V Symptom scales revealed an endorsement of symptoms that no longer meet criteria for Oppositional Defiant Disorder or any of the ADHD subtypes with the Conners ADHD Index falling to only 64%.
| Conners Parent Rating Scales (t-scores) | |||||
| Content Scales | DSM-IV-TR Symptom Scales | ||||
| Baseline | Post Rx | Baseline | Post-Focus System Rx | ||
| Inattention | 86 (very high) | 58* | Inattentive ADHD | 87 | 58 |
| Hyperactivity/Impulsivity | 84 (very high) | 63* | Hyper/Impulsive ADHD | 76 | 62 |
| Learning Problems | 81 (very high) | 47* | Conduct Disorder | 54 | 44 |
| Executive Functioning | 87 (very high) | 48* | Oppositional Defiant Disorder | 76 | 61 |
| Defiance/Aggression | 60 (high average) | 51* | Conners ADHD Index | 99% | 64% |
| Peer Relations | 48 (average) | 44 | |||
* Higher t-scores reflect greater level of impairment
* Improvements of well over one standard deviation
At baseline, N’s mother’s responses on the Comprehensive Executive Functioning Inventory (CEFI) resulted in a full scale standard score of 73 (low average range), reflecting an overall level of executive functioning that fell below expectations based on his average level of intellectual abilities. With the exception of flexibility, his mother’s observations produced scores that fell below expectations in all areas with particular difficulties in emotional regulation and working memory and a specific relative weakness in organization abilities. Post treatment, N’s full scale score significantly improved from the low average to average range. All of his scores had a positive trend in comparison to baseline with statistically significant improvements being seen in the areas of attention, emotional regulation, inhibitory control, organization, planning, and working memory.
| Comprehensive Executive Function Inventory (CEFI) | |||
| Baseline | Post Rx | Significance | |
| Full Scale | 73 | 98 | Increase |
| Attention | 73 | 107 | Increase |
| Emotional Regulation | 69 | 98 | Increase |
| Flexibility | 106 | 100 | No Change |
| Inhibitory Control | 70 | 97 | Increase |
| Initiation | 83 | 91 | No Change |
| Organization | 62 | 94 | Increase |
| Planning | 80 | 100 | Increase |
| Self-Monitoring | 82 | 90 | No Change |
| Working Memory | 67 | 104 | Increase |
*Lower scores reflect greater deficits
Summary of Changes:
N demonstrated significant improvements over the course of treatment, particularly in the areas of sensory-motor integration, executive functioning, working memory, oral fluency, and pseudoword decoding. External correlates of his improvements include a significant decrease in oral sensory seeking, a resolution of his drooling, significant decreases in hyperactive behavior and emotional dyscontrol, and significant improvements in classroom and academic performance.
N’s performance on measures of academic achievement revealed notable improvements in his grasp of phonics (25-points; <1.0 to 2.7 grade level), oral reading fluency (13-points; <1.0 to 1.9 grade level) and spelling (12 points; 1.0 to 2.1 grade level). With the exception of writing fluency, N’s performance in these areas is now generally consistent with or above his grade level. Cognitively, in comparison to baseline performance and ratings N has demonstrated significant improvements in visual response time and numerous aspects of executive functioning (e.g., attention, organization, planning, working memory).
Although N continues to demonstrate sensory seeking behaviors, his mother’s post-treatment observations suggest a significant improvement in N’s sensory threshold, which now fall in the typical range. External correlates of N’s improvements include a significant decrease in oral sensory seeking, a resolution of his drooling, significant decreases in hyperactive behavior and emotional dyscontrol, and significant improvements in classroom and academic performance. His emotional outbursts were also alleviated and he began to get along better with his brother. Not surprisingly, these changes resulted in more adventurous and socially competent behavior.
Comments by Ron Minson, MD, Unyte-iLs Clinical Director:
Well, it appears as if N has “grown a new frontal lobe” in a short five months! His main areas of improvement – “attention, emotional regulation, inhibitory control, organization, planning, and working memory” – are the hallmarks of frontal lobe function. The Focus System and CBT are an excellent combination for a case like this: the Focus System: Sensory Motor program working from the bottom up to improve the processing of sensory information before it reaches the cortex, CBT working from the top down. With improved subcortical processing, the higher centers are freed up to better perform executive functions.
There is also direct input into the frontal lobes from the auditory pathways as well as from the cerebellum and basal ganglia. These structures are intimately involved in frontal lobe and executive function. The beauty of this Focus System/CBT approach is the combination of a neurological intervention (Focus System), with a primarily cognitive one (CBT).
I want to thank the presenters for such a clear presentation of the history and pre/post therapy measures. Many of the improvements were two-year jumps in academic and cognitive performance within a five-month course of therapy. Pointing out the external correlates that indicate how the improvements in test measures are reflected in improved real world behaviors makes this case presentation all the more meaningful.


 © 2025 Unyte Health US Inc.
© 2025 Unyte Health US Inc.