Author:
Nikki Gomez, MOT, LOTR, NeuroTherapy Specialists, Baton Rouge, LA
Subject:
“K” a 12-year-old boy with attention, motor and social difficulties
Abstract:
K is a seventh-grade student, who presents with deficits in attention, coordination, social communication, and emotional regulation. His parents described concerns in his ability to verbalize his thoughts, to independently complete work and manage his emotions. They also observed motor tics and poor gross motor coordination. The iLs Program was completed as a home program with in-clinic treatments every other week. The iLs Concentration and Attention Program was 5 months.
Pre- and Post-testing measures were taken using informal and formal testing measures; client and parent interview, clinical observations, iLs Checklist and the Bruininks-Oseretsky Test of Motor Proficiency. Significant gains were seen in all measures.
After three consecutive years of using stimulant medications to control the symptoms of attention deficit disorder, K’s parents are relieved to no longer rely on medication; K is making honor roll with A’s and B’s. K’s parents also report progress in multiple areas, including his ability to complete school work without their assistance, confidence in expressing ideas in conversation, overall control of his body and greater participation in school.
Background:
As an infant and toddler, K had reoccurring ear infections until age 3 when pressure equalizing tubes were implanted. Per parent report, K has not had any other illnesses, injuries or hospitalizations.
K’s second grade teacher referred him for testing related to difficulties in the classroom. A Psycho Educational Evaluation revealed moderately atypical range for behavioral inattention and recommended that he be observed for further evidence of attention deficit disorder. At that time, an individual education plan was implemented which provided accommodations such as repeated directions, redirecting attention, and preferential seating. Later, he was diagnosed with ADHD and Asperger’s syndrome. He was prescribed medication for the ADHD.
Presenting Problems & Findings:
- Below average manual dexterity and ability to coordinate movements of his body in a quick and controlled manner
- Below average balance especially with vision occluded
- Poor motor skills resulting in avoidance of group sports
- Decreased attention to task, fidgeting, and impulsivity which required medical management through medication in order to participate in academic tasks
- Difficulty with emotional regulation described as ‘moodiness’ by parent report
- Decreased social skills with reports of lack of participation in conversation, decreased verbal expression of ideas and opinions
Therapeutic Goals:
- Increase ability to focus and attend without the need for medication
- Improve overall body coordination
- Improve management of emotional regulation
- Decrease the intensity of obsessive interest and repetitive routines
- Improve social interactions with peers and family
- Decrease motor tics and fidgeting
iLs Program Used:
- Concentration and Attention Program beginning August 19, 2014, and concluding on January 29, 2015. Bone conduction was gradually increased from 0 to 1.0 with 1.0 reached by the 12th session and consistently used until the conclusion of the program.
- Playbook activities were completed throughout the program although with various visual motor exercises such as tennis. The balance board was used consistently due to the significant impairments in balance observed at initial evaluation.
Other Interventions Used:
- K participated in swimming practice 2-4 times a week for 1 ¼ hour sessions through the duration of the iLs Program.
Summary of Changes:
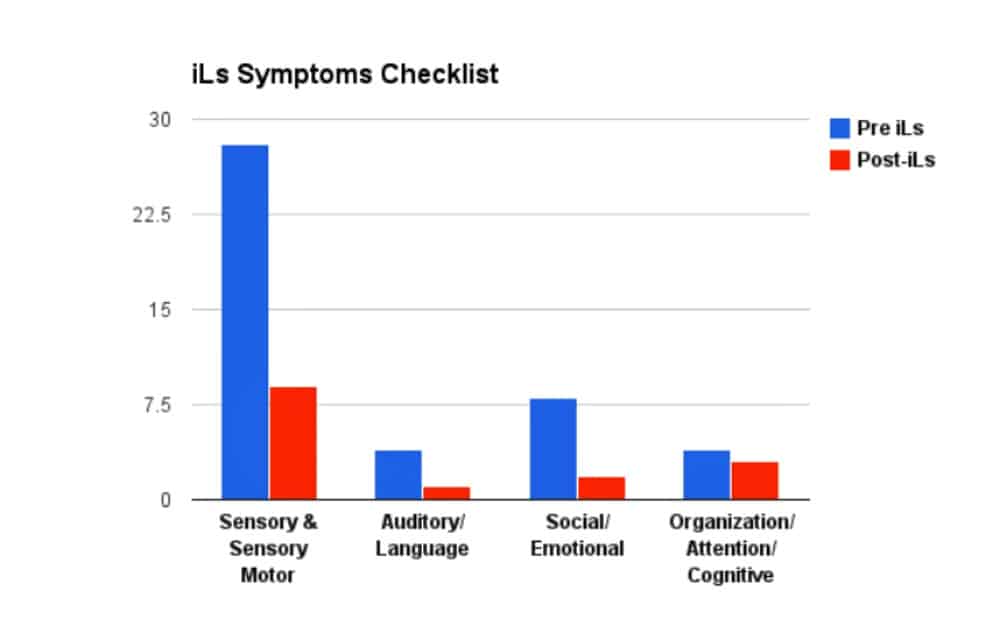
The iLs Symptoms Checklist was used to assess the changes in symptoms before beginning and after completion of the iLs Program. A lower score indicates a reduction in symptoms, i.e. improvement.
The significant changes in the iLs Checklist scores translated to his improved performance in school, ability to interact with classmates and participate in extracurricular activities.
| Bruininks-Oseretsky Test of Motor Proficiency (BOT2) | Pre-iLs | Post-iLs |
| Manual Dexterity | Below Average | Average |
| Scale Score: 8 | Scale Score: 13 | |
| Age Equivalent: 8:3-8:5 | Age Equivalent: 10:3-10:5 | |
| Upper Limb Coordination | Above Average | Below Average |
| Scale Score: 22 | Scale Score: 9 | |
| Age Equivalent: 16:6-16:11 | Age Equivalent: 8:3-8:5 | |
| Bilateral Coordination | Average | Average |
| Scale Score: 15 | Scale Score: 19 | |
| Age Equivalent: 10:9-10:10 | Age Equivalent: 12:0-12:5 | |
| Balance | Below Average | 50% |
| Scale Score: 6 | Scale Score: 15 | |
| Age Equivalent: 4:10-4:11 | Age Equivalent: 10:9-10:11 |
The Bruininks-Oseretsky Test of Motor Proficiency (BOT2) is an individually administered standardized test that assesses motor functioning of children. Subcategories of the complete form were performed as a tool to identify specific areas in which K may have limitations.
In six months’ time, K had improved 2 years in manual dexterity, one year and 3 months in bilateral coordination, and 6 years in balance. It was noted that K’s upper extremity score declined significantly. The upper limb coordination subset is comprised of 7 tests in which the child catches, throws, and dribbles a tennis ball. At the initial testing, K scored a perfect score of 39 raw points whereas at the reassessment date, K missed 6 points decreasing his raw score to 32 points resulting in decreases his standard score. Follow-up testing will be completed to further validate K’s motor performance abilities.
Video Discussion:
The videos display the motor changes observed in K before and after the iLs Program. The first set of videos show K standing on one leg with eyes closed. With vision occluded, K demonstrates initial effectiveness of the proprioceptive receptor’s information and vestibular system’s registration. Proprioceptive receptors are located in the joints and muscles throughout the body. These receptors send sensory information from the body to the brain about one’s body position in space. Once the vision information is eliminated by closing his eyes, the accuracy of the proprioceptive information becomes evident. As you can see, K displays very poor balance when his vision is occluded demonstrating the significant reliance on the visual system for awareness of his position in space rather than the positional awareness given by the proprioceptive and vestibular systems. Looking at the post testing video, K is observed to have increased postural control and sustained balance.
The second video pair demonstrates continued improvements in K’s balance even when demands are increased to standing on a balance beam in a tandem stance. Again, K is observed to have increased stability and control throughout his body as demonstrated by minimal postural sway from the initial midline position.
Parental observations and comments:
- “K had previously attended social skills training and had made good improvements. Although there was still room for progress, we were not focused on his social skills when we began iLs training. Now, we notice that K has more confidence. We can tell when he gives his opinions and how well he participates in conversations. He speaks openly without the anxiety of wondering what people are thinking about him. We were pleasantly surprised to see those improvements!”
- “When we began the program, K was very unbalanced. He was awkward with his arms when he walked and ran. Now, when he gets out of the car and is walking away to school, I can tell a difference in his walking. He has more control of his body and you can tell his overall coordination is better.”
- “I was very scared to take him off medication because I did not want his grades to drop. Nonetheless, we decided to take him off the medication and try iLs. It worked perfectly. He still has the same grades!”
- “Last year he did not want to join clubs, but this year he brought the Beta Club form to me wanting to join. The school personnel have noticed that he has increased his participation in academics and extracurricular activities. I talked with the physical education teacher the other day, who said K was doing wonderfully in PE class.”
Conclusions And Recommendations:
Overall, K demonstrates significant changes in many areas. In the area of social/emotional functioning, K has significant improvements in his socialization, often initiating participation in conversation and adding new ideas and opinions.
Per the parent report, K is able to “balance school stress,” demonstrating decreased feelings of frustration and more emotional control. Now K is independently completing homework tasks in an efficient manner whereas last school year he required significant parent involvement. K says he has increased ability to recall ideas while working, which results in faster work completion.
During the past three years of school, K required stimulant medications to remediate his decreased attention, impulsivity, and motor tics. When K began the medications, his parents noticed a decrease in the frequency of his motor tics. Currently, though he is not taking any medication, his motor tics have almost completely disappeared. This year, K has received all As and Bs and made Honor Roll.
Comments by Ron Minson, MD, iLs Clinical Director:
This professionally presented case provides the opportunity to highlight two areas in which iLs is particularly effective in improving brain/body organization and, consequently, improved therapeutic outcomes when combined with clinical expertise (in this case, occupational therapy) . First is the improvement in attention that resulted in removal of the ADHD diagnosis and successful performance without stimulant medication. Brain imaging studies show the problem in ADHD to be under activation of the right fronto-temporal (FT) areas of the brain. iLs improves activation of this area by stimulating the production of dopamine, a neurotransmitter essential for activation of the frontal lobes. Dopamine is produced by structures deep within the brain called Basal Ganglia (BG). Motor and balance board activities along with bone conduction innput stimulate the BG to release dopamine, making sustained attention possible.
Stimulants, such as Ritalin, artificially increase dopamine, but can have negative side effects requiring discontinuation or switching medication, as was the case with this youngster. They must be taken regularly for continued effectiveness; K had been on stimulant medication for 3 years before iLs. The experience that K was able to sustain attention without stimulant medication has been confirmed time and again by iLs practitioners.
The second area to emphasize is the role of the cerebellum in improving not just balance, coordination and fine motor control but also improving higher cognitive skills. I have written before about the role of the cerebellum in language, planning, emotional regulation and other cognitive skills. This time I want to direct you to a program on NPR that featured a 33-year-old man who was born without a cerebellum. Dr. Jeremy Schmahmann, a Harvard neuroscientist who has been studying the cerebellum for more than 30 years has some informative and entertaining things to say about this remarkable organ. Before going to that link to hear about the cerebellum in higher brain function, I want to underscore that all of the iLs activities have input into the cerebellum, improving its function and participation in brain/body organization. Of particular relevance are the following: using the balance board, bone conduction input, one leg standing, any and all things to increase proprioceptive input, coordinated motor activities, and cognitive challenges while doing the PlayBook activities, to name a few.
I enjoyed this comment from Dr. Schmahmann: “The big surprise from functional imaging was that when you do these language tasks and spatial tasks and thinking tasks, lo and behold, the cerebellum lit up”. Please enjoy the program on the cerebellum. And I offer my gratitude to the therapist for this informative presentation.


 © 2025 Unyte Health US Inc.
© 2025 Unyte Health US Inc.