– ENDING SOON –
The Care is Core Bundle
Discounted training and certification, an annual subscription, and Deb Dana come together to equip you with all the essentials to begin your journey as an SSP provider. Plus, receive a credit to the Unyte Care is Core Store to expand your professional library or self-care toolkit! Learn more →
“If you want to improve the world, start by making people feel safer.”
– Dr. Stephen Porges

Helps improve nervous system regulation in children and adults to support many symptoms and conditions.

Backed by clinical trials and real-world evidence, and informed by Dr. Stephen Porges’ Polyvagal Theory.

Enhances and accelerates the impact of other therapies, such as CBT, EMDR, SE, IFS, and neurodevelopmental treatments.
How does the Safe and Sound Protocol work?
The music of the SSP has been filtered through a patented, evidence-based algorithm that highlights specific sound frequencies that help regulate the autonomic nervous system and stimulate the vagus nerve.
Repatterning the nervous system through listening.

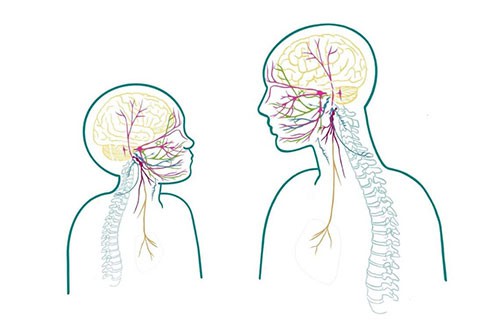
Humans need social connection. We look for cues of safety in other people by reading their faces, body language and tone of voice.
Some people, including adults and children who have experienced really difficult life events, are living with illness or injury, have sensory, learning or developmental differences, such as autism, or for many other reasons, may miss or misinterpret these cues as threatening.
Their autonomic nervous system may be biased toward experiencing the environment as unsafe, which can limit the body’s ability to heal and recover.
Auditory processing is a window into the nervous system. By listening to the specially filtered music of the Safe and Sound Protocol (SSP) in the context of a therapeutic relationship, the nervous system can be repatterned to better perceive calming frequencies, enhancing autonomic regulation by changing the way it responds to cues from the environment.
The SSP helps to regulate the autonomic nervous system and improve auditory processing, leading to better social connection.
When we experience the world as safe, we can more effectively and efficiently use our internal resources to support health and well-being, building the foundation for awareness, embodiment and resilience.

Humans need social connection. We look for cues of safety in other people by reading their faces, body language and tone of voice.
Some people, including adults and children who have experienced really difficult life events, are living with illness or injury, have sensory, learning or developmental differences, such as autism, or for many other reasons, may miss or misinterpret these cues as threatening.
Their autonomic nervous system may be biased toward experiencing the environment as unsafe, which can limit the body’s ability to heal and recover.

Auditory processing is a window into the nervous system. By listening to the specially filtered music of the Safe and Sound Protocol (SSP) in the context of a therapeutic relationship, the nervous system can be repatterned to better perceive calming frequencies, enhancing autonomic regulation by changing the way it responds to cues from the environment.
The SSP helps to regulate the autonomic nervous system and improve auditory processing, leading to better social connection.
When we experience the world as safe, we can more effectively and efficiently use our internal resources to support health and well-being, building the foundation for awareness, embodiment and resilience.

What this means for you and your clients:

Providers report that the SSP “opens up” their clients and relaxes their defenses, improving accessibility.

As a result, clients often experience quicker progress, becoming more engaged in therapy.

The SSP helps accelerate results and improve therapeutic outcomes.

Once integrated, the SSP often becomes an essential part of a clinical approach.
Impactful, long-lasting results for your clients are possible.
The Science of Safety
Explore the science behind the Safe and Sound Protocol
The autonomic nervous system controls the body’s most essential physiological processes, including heart rate, breathing, digestion, and bowel and bladder function. These systems are primarily working automatically, beyond conscious awareness or control. Autonomic state is guided primarily by the vagus nerve (CN X), which serves a key role in communicating information between the brain, body and environment.
Neuroception (different from perception) is a subconscious process of the nervous system in which it evaluates cues from the environment as safe, dangerous or life-threatening. The balance of these cues triggers a corresponding autonomic response, which influences how we feel, think and connect with others.
Auditory processing is the receipt, integration and interpretation of acoustic energy, and is closely linked to other sensory, central and autonomic nervous systems.
Accurate and discriminatory perception of sound is dependent on the function of the middle ear muscles, which tighten the tympanic membrane (eardrum) to support the perception and attenuation of certain frequencies. The middle ear transfer function is connected to a network of cranial nerves that contribute to the integration of sound with other sensory inputs in the brainstem, leading to cognitive, behavioral and physiological responses. The auditory processing system is a portal that fundamentally changes the way we experience and respond to the world.
The social engagement system is an integrated system of cranial nerves and structures of the face and head that enable social behaviors like facial expressions, head-turning, speaking and listening, alongside coordinating essential functions like swallowing, chewing, nursing (infants) and regulation of the heart and lungs. This system has a bidirectional relationship with the cortex and brainstem, where sensory information converges and is processed from the internal and external environment. Through the lens of Polyvagal Theory, the social engagement system evolved to enhance the ability to communicate, collaborate, and build trusting relationships with others from a neurological foundation of safety.

Tunes that retune.
The SSP uses a wide variety of music, including some that you may already be familiar with. All the music in the SSP playlists are thoughtfully sequenced and filtered through the patented, evidence-based algorithm backed by decades of scientific research.
This visual shows full-spectrum sound frequencies in a typical unfiltered clip of popular music.
Here is the exact same clip — after being filtered through the SSP’s algorithm.
What does the music sound like?
The SSP contains several vocal and non-vocal music playlists and levels of filtration to help you support client engagement and participation in the listening process. Multiple vocal and non-vocal playlists allow the SSP to be accessible to many populations, and allow you to customize delivery for your client.
This visual shows the frequencies of vocal music, filtered through the SSP’s algorithm.

This visual shows the frequencies of equally impactful non-vocal music, filtered through the SSP’s algorithm.
Everyone can benefit from
nervous system regulation.
nervous system regulation.
The SSP is suitable across the lifespan, and has been designed to complement a variety of therapeutic approaches and modalities.
SSP providers are psychologists, therapists, social workers, occupational therapists, speech therapists, school counselors, and more.
The SSP may be helpful in reducing symptoms and supporting overall health and resiliency for people seeking support for:
- Depression and anxiety
- Neurodevelopmental differences, such as autism, hyperactivity and attention
- Learning difficulties
- Auditory and other sensory processing differences
- Trauma history
- Sleep
- Neurological changes
- Other challenges related to autonomic dysfunction, such as eating difficulties, gut health, and more
It can be combined with and is supportive of other therapies, including:
- Neurodevelopmental treatment, such as occupational therapy, play therapy and sensory integration therapy
- Other forms of mental health and trauma therapies, such as Eye Movement Desensitization and Reprocessing (EMDR), Somatic Experiencing (SE), and Internal Family Systems (IFS)
- Cognitive behavioral therapy (CBT) and other forms of talk therapy (e.g. DBT, MCBT, etc.)
Experience the benefits of the SSP in your practice.
The SSP is trusted by these practitioners and professional organizations as part of their healing toolkit.






Together, clinical trials and real-world evidence create a powerful and holistic evidence base for Unyte programs.
Real-world evidence. Real change.
Discover the science behind the transformative power of the Safe and Sound Protocol. Explore real-world case studies demonstrating the wide-ranging impacts of nervous system regulation. View all Case Studies →
Clinical Trials
The SSP’s effectiveness has been proven in a wide range of clinical studies, including clinical trials involving children and adults with autism. View all Research →
Deliver from almost anywhere to anyone with the Unyte app.
Help more clients — easily and seamlessly
The SSP is delivered through a user-friendly app-based platform, compatible with Android and iOS devices.
Delivered either in-person or remotely, clients experience the SSP through over-the-ear headphones via the Unyte app. Providers have full control, and can manage client access, deliver listening sessions and monitor progress through MyUnyte, the intuitive platform.

“Safe, sound, and simple. The level of ease and simplicity that comes with SSP digital delivery contributes to keeping the experience within reach of the nervous system’s capacity to safely engage.”
— Deb Dana, LCSW
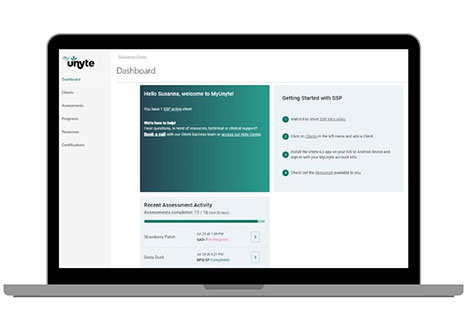
MyUnyte
An intuitive online client management dashboard. Create new accounts, choose SSP programs and pathways, and more in just a few clicks.
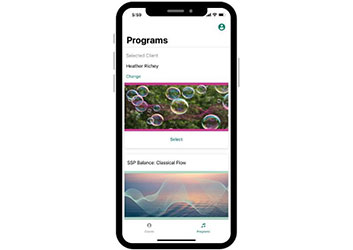
Unyte App
Facilitate all your clients’ listening through the Unyte app, available to both providers as well as clients for remote delivery.

Unyte Community
We’re here to support you! Webinars, technical and clinical support, resource articles, online communities, and more are available to all SSP providers as part of your subscription.
Get started today!
You must be a qualified professional to deliver the SSP. SSP Training and Certification covers both theory and the practical application of the Safe and Sound Protocol. Once certified, a subscription is required to deliver the SSP to your clients.
Annual Monthly Subscription
Pay monthly
$139/month
12-month subscription, billed monthly, auto-renewal.
+ $349 $249 one-time purchase of SSP Training and Certification
Annual Upfront Subscription
Pay annually and save!
$125/month
$1,499 today, billed annually, auto-renewal.
+ $349 $249 one-time purchase of SSP Training and Certification
Have questions? We’re here to guide you!
Book a free, personalized consultation or call us directly at 1-866-594-9453.
| What’s Included |
Start with Training Only |
Training and Subscription Bundle |
|---|---|---|
| Online, on-demand learning | ✓ | ✓ |
| Special pricing on SSP Training and Certififcation | ✓ | |
| Access to deliver the SSP after becoming certified | Subscription required before you can deliver the SSP | ✓ |
| Access to MyUnyte | ✓ | ✓ |
| Unyte Assessments and Unyte Resources | Limited | ✓ |
| Unyte app for in-person and remote delivery | ✓ | |
| Live and online support, including introductory provider meeting | ✓ |
| What’s Included |
Start with Training Only |
Training and Subscription Bundle |
|---|---|---|
| Online, on-demand learning | ✓ | ✓ |
| Special pricing on SSP Training and Certififcation | ✓ | |
| Access to deliver the SSP after becoming certified | Subscription required before you can deliver the SSP | ✓ |
| Access to MyUnyte | ✓ | ✓ |
| Unyte Assessments and Unyte Resources | Limited | ✓ |
| Unyte app for in-person and remote delivery | ✓ | |
| Live and online support, including introductory provider meeting | ✓ |
We’re Here To Help!
Discover how the Safe and Sound Protocol can create lasting change for your clients.













 © 2024 Unyte Health US Inc.
© 2024 Unyte Health US Inc.