The information presented in this case study was submitted by the identified provider and reviewed by the Unyte Clinical Team. Modifications to the text have been made solely for the purpose of enhancing comprehension and clarity for the reader’s benefit, and were carefully applied while ensuring the accuracy and integrity of the original submission. Unyte Health makes every effort to use updated terms and inclusive language, this case study retains the author’s original descriptions to be most sensitive to the client’s identity and preferences.
About the Provider
Name: Elvira Lidia Straus
Disciplines/credentials: Psychotherapist, SEP, Barbara Brennan practitioner
Modalities: Safe and Sound Protocol (SSP), Somatic Experiencing
Client Background
Name: Lisa (pseudonym)
Age and Gender: 49-year-old woman
Program Delivered: Safe and Sound Protocol (SSP) Connect (Hours 1-5); Core (Hours 1-5); Balance (Hours 1-5)
In 2023, Lisa experienced a tumultuous year in her professional and personal life. Self-employed, she worked as an oraculist and body educator. In June 2023, Lisa was anticipating an entrepreneurship class to boost her career. She had faced difficulty in her career a year prior when she had been ousted from a professional women’s group that she led. Lisa relied on this group for social support, so she felt unmoored and anxious about future social endeavors. The entrepreneurship class was intended to boost her confidence again. However, she ended up unable to attend the course after experiencing an unexpected trip to the hospital.
One night, Lisa woke up unexpectedly and “perceived an unfamiliar relationship with her surroundings,” a feeling she later characterized as derealization. Since this was her first experience with that sensation, Lisa went to the hospital. After a series of tests and a subsequent visit to a neurologist in the following weeks, Lisa was diagnosed with anemia and a vitamin B12 deficiency. They found no evidence of brain damage or any other critical issues. This was not Lisa’s first trip to the hospital in 2023. Prior to this incident, she experienced a moment in April when she felt a strong pressure in the back of her neck as well as hot flashes in her hands, feet and face. She went to the hospital that time as well, and an electrocardiogram revealed nothing conclusive.
Following her second hospital trip, Lisa sought out treatment at a local clinical school, which offered support for trauma and anxiety disorders. By August, she was referred to provider Elvira Strauss. Upon their initial meeting, Lisa cited a variety of symptoms as causing distress. These symptoms included a severe burning sensation in her head, inability to relax, shortness of breath, intrusive thoughts, memory problems, dizziness, fatigue, time blindness, and an inability to work due to perceived incompetence. This lack of autonomy in both her body and mind created a sense of powerlessness, fear and anger.
Prior to starting treatment with the Safe and Sound Protocol (SSP), Lisa and Elvira were able to work through some of her symptoms, leading to clear therapeutic goals. By February 2024, when Lisa began the SSP, she was experiencing some difficulty hearing out of her left ear and facial numbness that made her feel insecure when talking to others. Lisa “wanted her life back,” and she set the clearly defined goals of reducing the intensity of her physical symptoms and regaining the confidence to be in public spaces and social situations with less stress.
Implementation of the Safe and Sound Protocol (SSP)
Lisa initially began listening to the SSP with Elvira. After a few sessions of co-listening, she transitioned to independent sessions in her home.
During her listening, Lisa would sometimes walk through the park near her home. This would occasionally cause the music to buffer, so she resumed her sessions in her house. She also experienced some difficulty with her headphones during weeks 20-25 and 30-32.
Ultimately, she performed two complete cycles of SSP Core over the course of 36 weeks.
Response
After her first month of SSP, Lisa “reported greater confidence in being in public and engaging with people.” This was one of the primary reasons she sought out treatment, so it was relieving to Lisa to be able to ease back into socializing.
Initially, she did notice that her physical symptoms, such as the pain in her left side, would flare up more frequently after socializing. After six months, she adjusted the frequency of listening to the SSP, completing three or more sessions in a week. This created a significant improvement in her symptoms, and by the eighth month, she began having days without any symptoms at all. Provider Elvira noted that “it was as though she was feeling like herself again.”
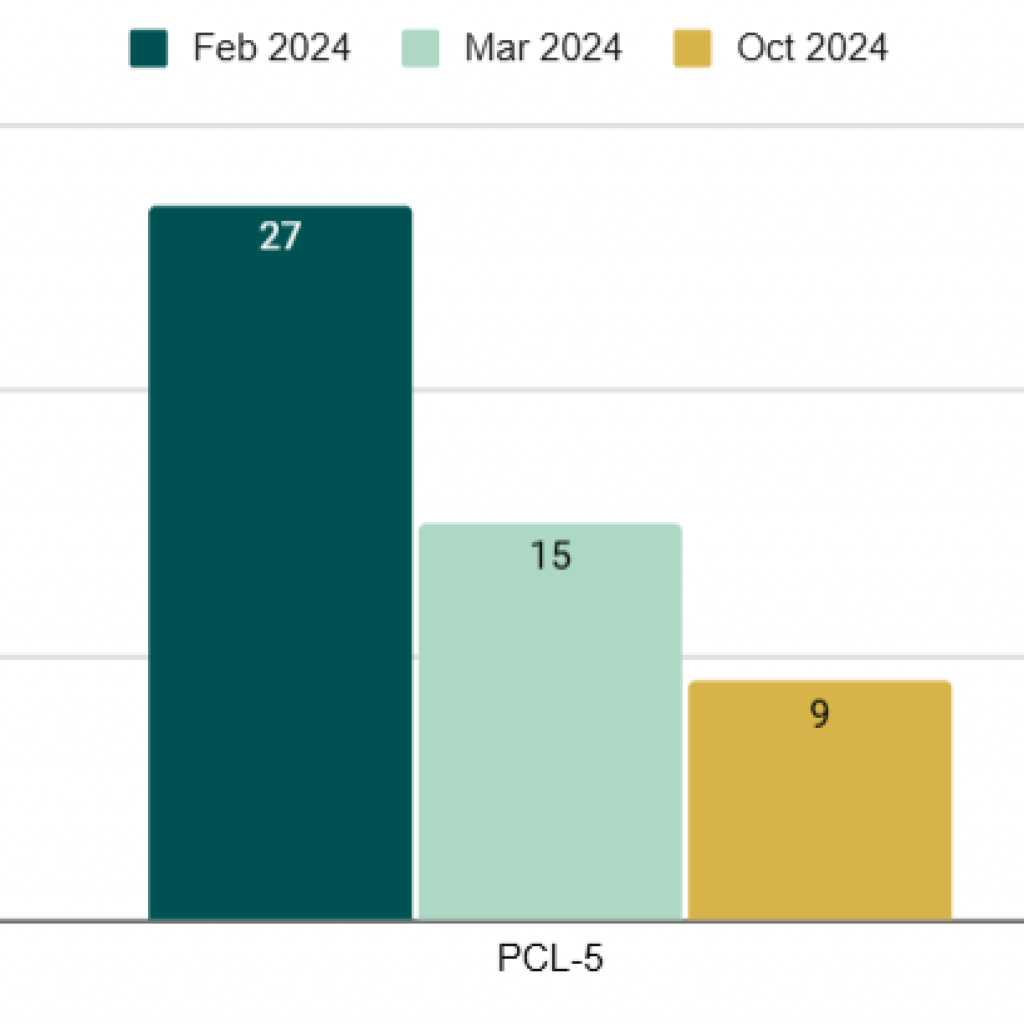
The graph above shows Lisa’s score changes on the PTSD Checklist for DSM-5 (PCL-5) after each round of the SSP. The PCL-5 is a 20-item self-report measure that can be used to monitor the presence and severity of PTSD symptoms over time. A change of 5-10 points is reliable, while 10-20 points indicates clinically significant change.
Discussion
Elvira noted that “the most noticeable change in [Lisa] was her expressiveness; her smile became more present and nuances in the expression of her emotions could be observed over the weeks since she began the protocol.”
Lisa had become more confident, feeling assured in her day-to-day choices. She returned to places and situations that she had previously gone out of her way to avoid, feeling more secure in her ability to face challenging situations. Her experiences in the past no longer prevented her from participating in daily life. Between her physical symptoms and anxiety about entering the world, Lisa had previously needed people to take care of her. This was no longer a necessity after treatment.
Lisa’s own preparedness and determination aided her significantly in her treatment. She also had established a trusting relationship with her provider prior to starting the SSP that made her trust Elvira’s recommendations, thus increasing the likelihood of treatment efficacy. Elvira encouraged Lisa to pursue treatment at her own pace, allowing Lisa to choose when and where she completed listening sessions. The SSP allowed Lisa to feel confident in her nervous system again, trusting the signals it sends.
Lisa faced numerous challenges during her therapeutic journey. Aside from technological issues, Lisa experienced a lack of support from her loved ones. Her family made frequent comments of “disapproval of her lifestyle and treatment,” turning family gatherings into sources of discomfort and criticism. She told Elvira that “a harmonious relationship with her family and eventual proximity to [them] would have to wait.” However, Lisa was also able to make new friends during this time period, proving she could establish a support network independently, which had felt unachievable just a few months prior.
One of the primary reasons that Lisa’s family disapproved of her treatment style was her refusal to start psychiatric medication. Feeling unheard and not taken seriously by the medical practitioners at the hospital, Lisa did not heed their advice to seek out a psychiatrist. Her family dismissed this as irrational, but Elvira listened to Lisa’s concerns and took her seriously. Elvira researched her symptoms and found information about Functional Neurological Disorder (FND), which often is dismissed by practitioners as attention-seeking or symptom-feigning since medical tests are inconclusive. When Elvira discussed this potential diagnosis with Lisa during week 33 of SSP treatment, Lisa was intrigued and felt supported by her provider. It helped them frame the rest of their treatment more effectively to help Lisa, allowing her to feel more relief from her symptoms and take more control over her life again.



 © 2025 Unyte Health US Inc.
© 2025 Unyte Health US Inc.