| By Unyte Editorial Team Reviewed by Unyte Clinical Team |
May is Mental Health Awareness Month, and this year’s theme, “Where to Start,” poses an essential question for providers: where do I begin when supporting my clients? With a wide range of modalities and therapeutic approaches available, finding the best method for your client can be daunting, especially when there isn’t a one-size-fits-all solution.
In this blog, we’ll explore the benefits of a “bottom-up” approach in therapy, informed by Polyvagal Theory, and practical tools like the Safe and Sound Protocol (SSP). These methods offer providers a valuable lens to healing that can be applied within an existing practice to help accelerate clients’ progress in treatment and enhance outcomes to support overall mental health and well-being.
Bottom-Up vs. Top-down Approaches
Therapeutic modalities that focus on addressing client needs cognitively are referred to as “top-down” therapies. This approach relies on assessing conscious thought patterns, communication, problem-solving and decision-making processes to address psychological challenges and often involves talk-based interventions.
Bottom-up therapies, on the other hand, target the body’s physiological and emotional states rather than cognitive processes. These approaches are based on the science behind emotional regulation, trauma and other psychological presentations being rooted in the nervous system.
There are a few reasons a bottom-up approach may be more effective for some clients:
Addresses Deeper Issues
Bottom-up approaches can be more effective than top-down approaches in targeting issues connected to physiological and neurological processes. By addressing disruptions in the autonomic nervous system, such as those caused by trauma, sensory processing differences and neurodevelopmental differences, bottom-up methods can provide support that cognitive interventions alone may not fully achieve.
Strengthens the Body-mind Connection
Bottom-up therapy emphasizes the critical role of the body — specifically the nervous system — in overall well-being. By considering physiological responses often linked to emotional and psychological states, this approach can help create a safe space for brain and body integration and healing to achieve impactful, long-lasting results.
Helps Support Emotional Regulation
For clients experiencing high levels of stress, anxiety or trauma, bottom-up techniques can be more effective in promoting emotional regulation. By targeting the nervous system, these interventions can help create a sense of safety and calm within the body, which can also be supportive of top-down, cognitive work.
Engages Beyond Rational Thought
Top-down therapies assume that clients can use rational thought processes to control their emotions and behaviors. A bottom-up approach can be particularly beneficial for clients with trauma or severe anxiety who may struggle to engage in rational thinking when their autonomic nervous system is dysregulated.
Accessible for Diverse Client Populations
Bottom-up therapies do not require clients to articulate their thoughts and feelings clearly, making them accessible to clients with language difficulties. This can especially benefit clients with sensory processing differences or autism, who may experience heightened sensitivity to sensory inputs, and be unable to communicate.
Understanding Polyvagal Theory
Dr. Stephen Porges’s Polyvagal Theory provides insights into how the nervous system influences emotional and psychological states. This revolutionary perspective on how the body responds to stress highlights the role of the vagus nerve in regulating stress responses and social engagement, categorizing the nervous system into three states:
Safe and Social State (Ventral Vagal)
The ventral vagal state promotes calmness, connection and positive social interactions through the activation of the social engagement system. When we can access this state as a response to cues of safety, we are more able to socially interact and co-regulate with others around us.
Fight-or-flight State (Sympathetic)
In this state, the ventral vagus withdraws, and we experience heightened alertness in response to perceived threats. The sympathetic nervous system functions like a gas pedal, mobilizing internal resources in response to danger. Symptoms include an increased heart rate, fast and shallow breathing, tension in the neck and shoulders, and anxiousness. This is the body in survival mode.
Shutdown or Immobilization State (Dorsal Vagal)
The dorsal vagal state activates when our nervous system detects extreme danger, leading to feelings of helplessness or dissociation. This state is the body’s natural response to overwhelming stress and trauma. Symptoms may include chronic fatigue, dissociation, numbness and depression, which can prevent progress in the healing process.
The dorsal vagal state can also have restorative properties when our nervous system experiences safety, including experiences of meditation and tranquility.
Polyvagal Theory acknowledges the role of the nervous system in creating a foundation of safety. For many clients, it’s not a matter of choosing a top-down approach or a bottom-up approach, but integrating both into an effective treatment plan.
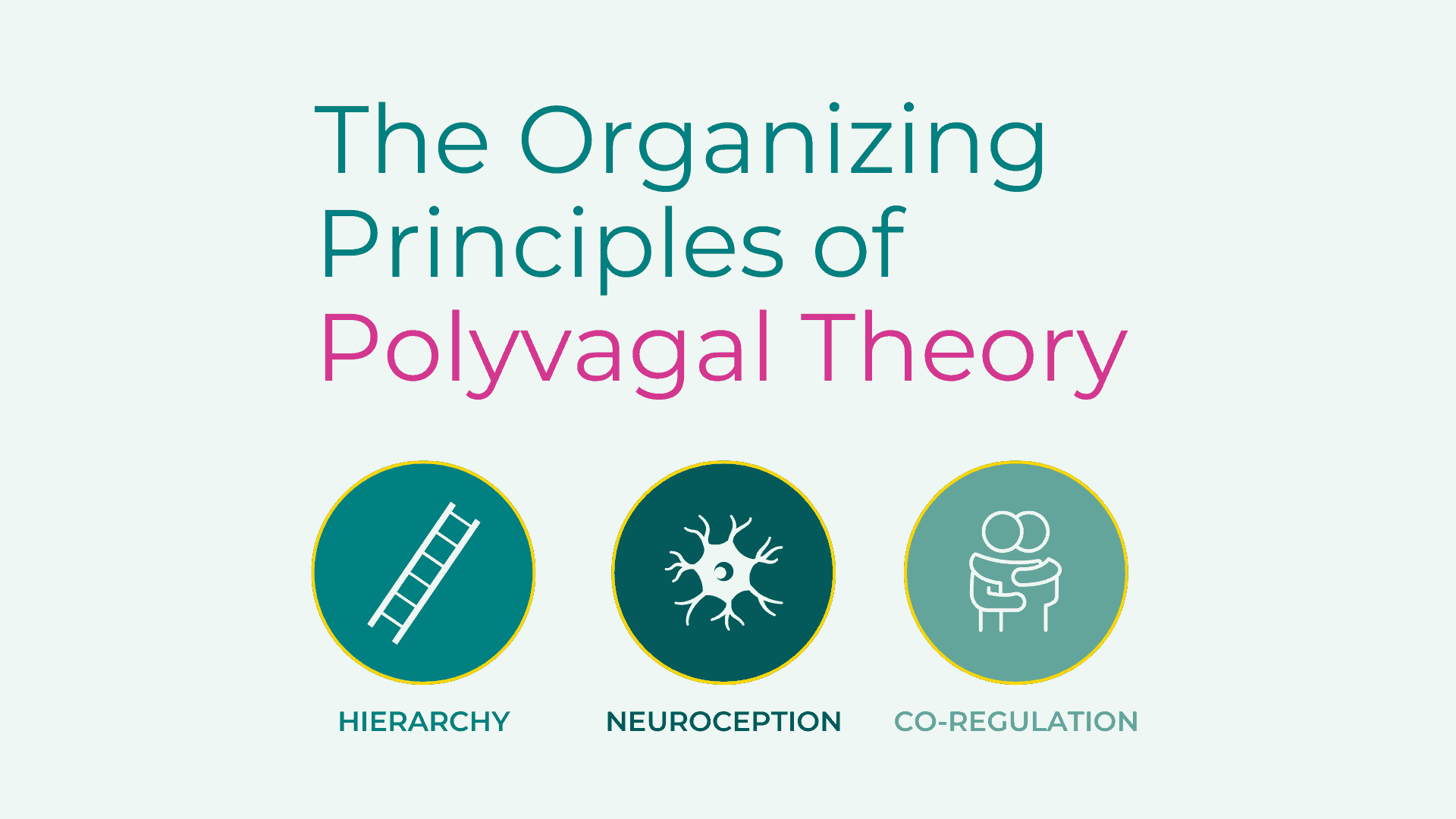
Free download: The Organizing Principles of Polyvagal Theory
Share with your colleagues and clients! The science of safety explained visually in an infographic format.
Using the Safe and Sound Protocol (SSP) as a Practical Application of Polyvagal Theory
The SSP is a listening therapy that uses specially filtered music to stimulate the vagus nerve, sending cues of safety to the autonomic nervous system. The patented algorithm highlights frequencies within the music that are similar to the human voice.
Real-world evidence has shown that the SSP is an effective tool in supporting clients experiencing symptoms related to anxiety, depression and trauma. Highlights of evidence collected from existing SSP providers include:
- Anxiety: 61% of clients moved from clinical to non-clinical levels, with a 5.6-point improvement in symptoms.
- Depression: 54% of clients transitioned to non-clinical levels, with a 5.4-point improvement in symptoms.
- Trauma: 63% of clients experienced significant reductions in trauma-related symptoms, with a 17.5-point improvement overall.
The SSP enhances auditory processing, reduces sensitivity to background noise, and fosters social engagement, making it a powerful tool for clients with anxiety, trauma, and sensory processing differences. Studies published in peer-reviewed academic journals, including the Harvard Review of Psychiatry, Music and Medicine, and the International Journal of Environmental Research and Public Health, demonstrate its effectiveness in supporting clients with Functional Neurological Disorder (FND), voice and throat complaints, and autism.
When it comes to therapy, there is no universal approach. While top-down therapies may be effective for some, incorporating bottom-up therapies for a more holistic approach can better support clients and accelerate outcomes. With Polyvagal Theory and the SSP, therapists can create a comprehensive toolkit to support their clients. These innovative approaches, supported by real-world evidence, offer therapists new ways to address mental health issues effectively.



 © 2025 Unyte Health US Inc.
© 2025 Unyte Health US Inc.