When your child is referred to an Occupational Therapy evaluation, there can be a lot to take in.
Where do you get the referral? What does it all mean? What’s next?
We’ve outlined the process for you so you know how to prepare, what to expect and which questions to ask so you and your family get the most out of your evaluation.
Physician referral:
Before an Occupational Therapy evaluation is scheduled, a physician’s referral is typically required. This referral usually comes from your pediatrician, family physician or neurologist. The referral may be given to you to choose a therapist or facility, or your doctor may fax it to a recommended clinic. The referral may be for problems with:
- delays with fine motor skills
- sensory integration
- self-care skills
- emotional or behavioral dysregulation
- handwriting
- learning differences
- visual perceptual and processing skills
- or developmental delays
“Developmental delays are commas, not periods. Your child can still get there.”
Paperwork:
Now that you have a referral from a physician, what’s the next step?
When you first visit a therapist, they’re going to ask for your insurance information. This allows the therapist to determine your co-pays or private pay fees and your visit cost.
You will also complete an intake form. Ask your facility if they have an online form on their website, which might save you time during your visit.
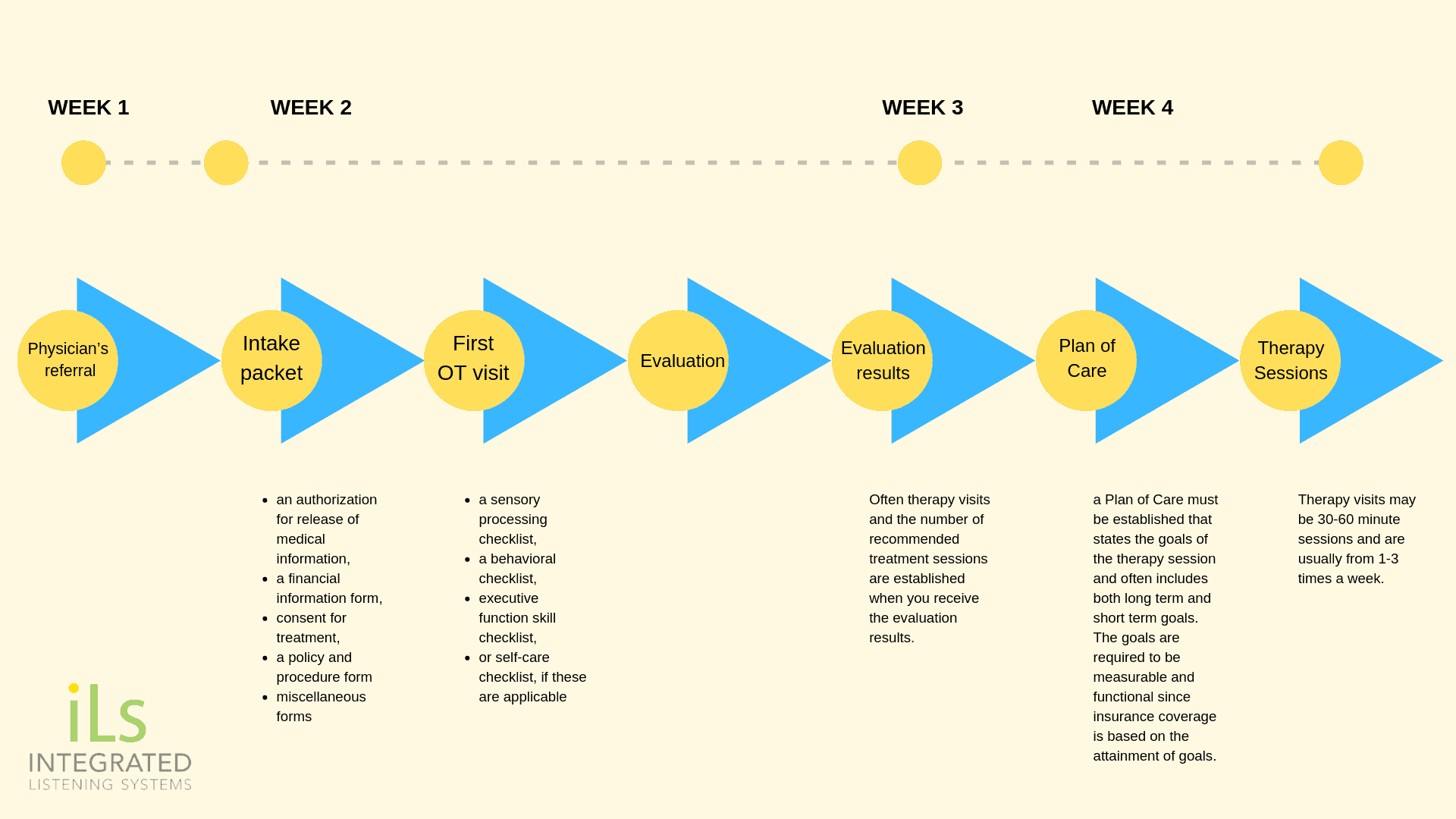
Often you will be given a packet of forms to complete: an authorization for release of medical information, sign a financial information form, consent for treatment, and a policy and procedure form. The contents of this packet vary among therapy offices.
Appointment:
Once all the information has been completed, you will set an appointment with your Occupational Therapist.
You thought you were done with all the forms. Not quite yet. 🙂
Sometimes additional forms will be requested prior to the visit such as a sensory processing checklist, a behavioral checklist, executive function skill checklist or self-care checklist, if these are applicable. Often, parents are invited to observe during the evaluation, especially if there are behavioral concerns or the child is young.
Meet your therapist. Bring a list of your concerns and any questions you have so you can be sure to get the answers you need on your first visit. This is a good practice to form for each visit with your Occupational Therapist so everyone is on the same page with therapy goals and any obstacles.
Evaluation:
Your therapist will determine a baseline for abilities; an evaluation.
Many therapists perform play-based evaluations that are both standardized and involve clinical observations with the child performing functional skills such as:
- ball play
- fine motor play
- visual motor tasks
- visual perceptual skills
- gross motor tasks
- self-care (such as dressing, shoe tying, or eating if applicable)
- social interactions
- and sometimes visual processing skills
Often therapists use testing procedures based on the type of certifications they have received since some tests require additional training, ie:
- SIPT (Sensory Integration and Praxis Test)
- Beckman Oral Motor Test
- SOS (Sequential Oral Sensory) Approach
- or Irlen Syndrome Testing
The tests used may vary from one therapist to another. Therapy evaluations may last from one to two hours, depending on the facility.
Note: Sometimes the evaluation moves more smoothly if the parent is not in the room; if there is difficulty in the relationship or if the parent has a hard time just watching the child perform during a standardized test, it may be best for therapist to carry out the evaluation alone.
Results:

Often therapy visits and the number of recommended treatment sessions are established when you receive the evaluation results. Therapy visits may be 30-60 minute sessions and are usually from 1-3 times a week.
Before the first therapy session, a Plan of Care must be established that states the goals of the therapy session and often includes both long term and short term goals. The goals are required to be measurable and functional since insurance coverage is based on the attainment of goals.
Learn how some therapies can even be administered at home here.
Therapy visits:

Treatment sessions may include a wide variety of play and movement opportunities from swings, therapy balls, balance activities to writing tasks, and eye-hand coordination games.
The type of therapy depends on your therapist’s training and the therapeutic goals. There is a wide range of variability among pediatric Occupational Therapists that is based on the type of equipment used, experience of the therapist, specialized training and the practice model of the facility.
Many therapists use music and movement therapy to target therapeutic goals.
The Therapist:
Occupational Therapists are trained in medical diagnosis, developmental stages and research-based therapeutic interventions to improve the quality of life for children. They use exercises, play-based activities and adaptive equipment to help children become more independent for home, school or play. An OT may be seen in the school system, in early intervention (0-3 services), private clinics, outpatient or inpatient hospitals.
Remember that even if your child requires additional support from OTs or other medical professionals, this doesn’t mean they will stay in therapy for the rest of their lives. The earlier and more appropriate the intervention, the better and more permanent the gains.
What is iLs?
Integrated Listening Systems (iLs) works with numerous therapists across the globe, and has trained more than 10,000 therapists to use the Focus System in clinic and at home, which combines music and movement with cognitive exercises to improve brain function.
To learn more about iLs or find an iLs provider in your area, please contact us below.



 © 2025 Unyte Health US Inc.
© 2025 Unyte Health US Inc.